#RaiseYourHandStories
Share your story, save a life.
The Raise Your Hand Campaign collects stories from healthcare workers who have been victims of violence in the workplace. Our hope is that their words will raise awareness and inspire change. Share your story here
“My name is Linda, I have been a psych nurse both impatient and out pt. I have been attacked, punched, kicked,had cups of urine thrown on me. I have had 2 broken bones, have been strangled X3, have been picked up and thrown and stabbed in the ribs with a pencil. And that is just the physical wounds. Yes, I raise my hand. ”
“I was assaulted at work in local Level II ED. I was kicked in the back to the head by a homeless male patient while caring for him at the bedside, private room. Fortunately, I had removed his shoes on arrival. It was near the end of my shift. I was seen and treated in the ED, initial diagnosis was contusion and muscle spasms, went home. There was another nurse in the room. Said patient was being treated for sepsis, had received fluids and antibiotics, was alert and oriented x 3. He was not intoxicated and had negative tox screen.
I was not able to return to work for 2 1/2 months, worked light duty x 3 months. Am currently working regular duty, four hours only, half of my regular shift, remain on L & I. Charges were pressed. Assault occurred about 1430.
Am still in OT , counseling, seeing neurologist and occupational medicine on regular basis. I continue to have vision problems, had to change glasses and go to contacts with glasses, L & I didn’t pay a dime towards and because it was before a year was out on my own eye insurance, it was all out of pocket for me. I continue to have problems with light sensitivity, concentration, short term memory, emotional issues and other assorted issues common to post concussion syndrome. I have just had steroid injections into my neck. That is finally helping the continued head and neck pain have had since the November assault.
My recovery continues. My Occ Med and Neurologist are encouraged by the progress have made so far. My teenage sons, who I raise alone, as their Dad died 10/2017, not so much.
This is my worst assault. I have been kicked in the face, slammed against walls, punched, spit on, sworn at , slapped, and threatened to be killed-more than once. The last one who threatened to kill me was sent to jail, 1-2 years ago.
Have worked in this same ED since 1992. Have seen the behaviors of assault and abuse to nurses and staff escalate in the last ten years to intolerable levels. Have been known for my ability to calm people down, to talk people down, to encourage others. Now, am even more afraid to go to work. Talk someone down? I call security and stay away from them. Anyone , at any time, can kill me or any of my co-workers at work. Anyone, at anytime, can hurt me again, making daily living misery and pain.”
“ I remember several years ago working as the night charge RN in a suburban ER a patient came in screaming that if she did not get placed in a bed she was going to have a “seizure”. It was an extremely busy night and the rooms were full and the halls were lined with chairs and stretchers. The patient looked straight at me and said “I told you bitch” and started to throw herself on the floor and started to have what looked like seizure activity. Myself and 2 other staff members put her in a wheelchair which she promptly stopped her “seizure activity”. We were working to get another patient that was headed to the floor into a wheelchair to open a bed for her, I had just cleaned the bed and turned my back to walk past her to grab a sheet to put on the bed and the patient lunged at me swinging. The other staff member that was there pushed me out of the way so she did not make contact but was screaming and swinging.
Later in the night after her workup was complete and they were sending her out with police escort (because she had continue to verbally assault staff and threaten staff, as well as refuse to leave the property), as she was leaving with hospital police from the Emergency Room they passed me and she screamed “its all your fault, I am coming back for you bitch”
About 2 weeks later EMS (a crew that rarely comes to us due to distance) called in that they were bring in a patient for unwitnessed seizure activity but that the patient was alert and oriented. When they rolled in the patient from 2 weeks before was on the stretcher. I sent them to a bed and one of the medics lingered back and I asked him why since they chose to come so far and he said “she insisted she said she had to come here because she had unfinished business” I immediately notified our officers of the potential situation and sure enough when the primary RN went to triage the patient she started screaming that I needed to go to the room so she could kick my ass cause she had been looking for me for 2 weeks.
I am thankful that we were able to avoid physical assault with this particular patient on my encounters with her. However over the years I have seen her come in police custody because at some point she ended up in jail for assault charges, so someone as some point was assaulted by her.”
“I had given an injection to a patient who afterward grabbed the dirty syringe and needle and stabbed me in the hand. I also had a drunk patient strangle me until five staff members could pull her off of me- causing c5-6 injury. I was strongly told by management that it was bad PR to press charges.”
“ In my nursing career I have been punched, kicked, spit on, threatened, had my eardrum pierced by patients. I’m not sure what or who I’m most angry:
The violent patient who takes weeks to stabilize when repeatedly admitted, and the docs who hesitate to adequately medicate. The ‘system’ which does not fund adequate resources for patients. The overpriced medications prescribed but not affordable to our patients. The methamphetamines our patients consume inducing psychosis and unpredictable aggression rarely impacted by verbal de-escalation techniques. Lack of staffing and security personnel. ”
“It started like any other day. I got floated to another ICU, we were short staffed, I got a transfer from the medical floors. An alcoholic and meth user in fulminant withdrawal had been extremely aggressive and needed more medication to manage his withdrawal symptoms (frequently those going through withdrawal become aggressive and agitated). A safety sitter had been assigned for his and my protection. More patients were admitted, the decision was made to open another ICU and move my 2 patients to that unit. My safety sitter was pulled to watch a suicide attempt patient. I argued against moving my agitated patient twice in one shift.... medication was given to help sedate him, 4 point restraints were placed to keep me and him safe. We moved. His aggression and agitation worsened, more medication was given. We were short staffed and there weren’t any other nurses available to help. His aggression worsened. At some point he broke off a side rail. His 4-point restraints ripped. More were applied. I called for a security alert. Nearly 30 minutes later, 5 security guards, a broken bed, 3 sets of broken 4-point restraints, and enough medication to tranquilize an elephant, he stopped. Everything hurt. I could feel the places were the bruises would form over the next few days. My legs burned, tingled, and ached. My back seized. We were short staffed. I was asked to finish my shift. I went to the ER that night for an evaluation (which is something I rarely do, unless I feel like I’m ‘dying’). A back strain they said, take some ibuprofen and rest, follow-up with workman’s compensation in a couple of days. It took almost 3 hours to drive home because of the pain.
“It’s NOT a muscle strain,” I would tell the work comp doc, “my legs are BURNING, like I’m walking in broken glass and someone has lit my legs on fire at the same time!” I got an MRI. Disks were herniated and torn, ligaments torn, bones broken off. My spinal cord was severely compressed. I went for steroid injections. Then I lost bowel and bladder function. I went for surgery. A micro-discectomy turned into a macro-discectomy (over 90% of the offending disks were removed), a synthetic wouldn’t be placed and a fusion aborted because it wasn’t ‘pre-authorized’. Eight months later I returned to work. I don’t run. My feet don’t simultaneously leave the ground. I live in pain.
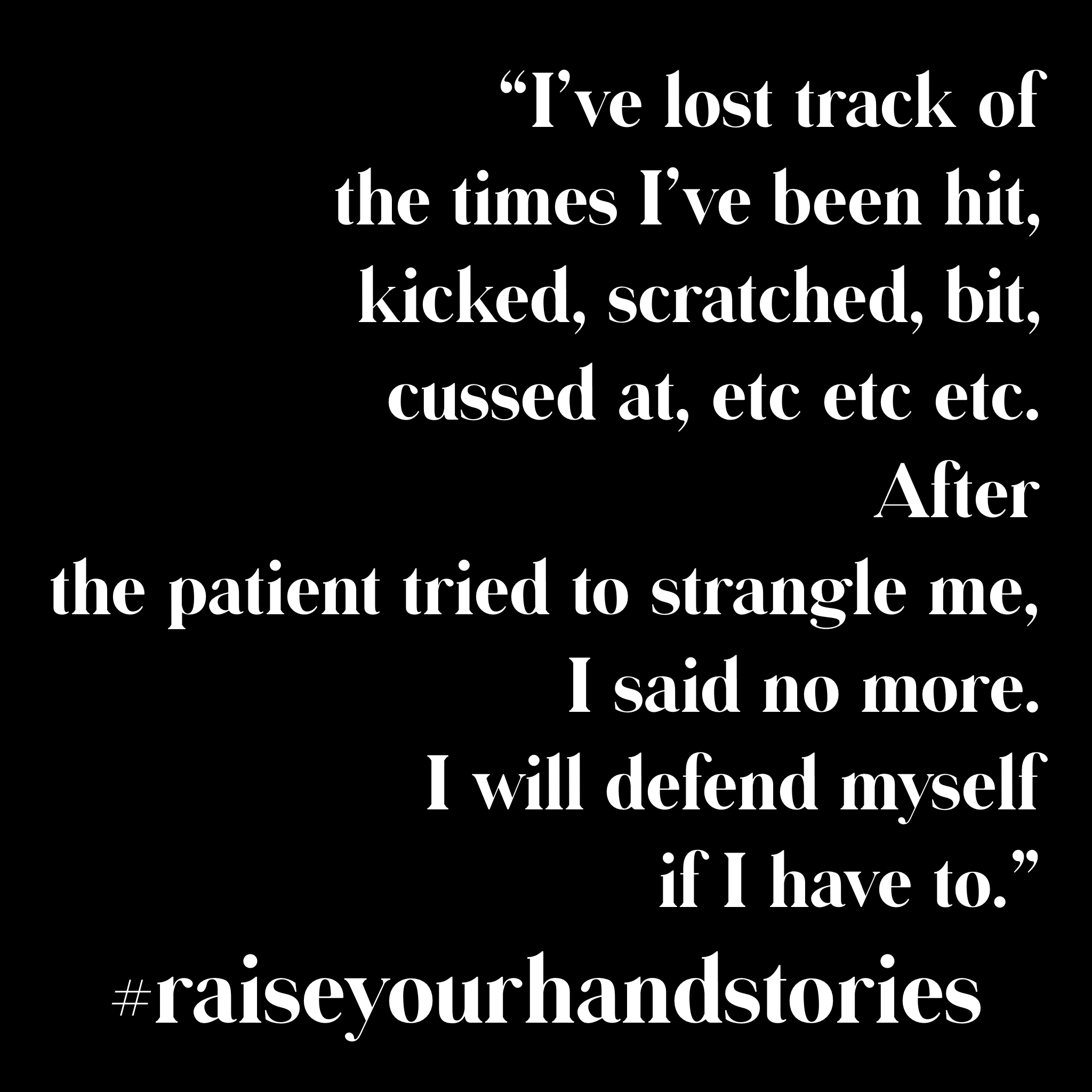
Throughout my nursing career I have had full urinals, surgical instruments, phones... thrown at me; been hit, kicked, bit, and spat on (with and without blood); I have been called entire dictionaries worth of colorful names. I still have PTSD when taking care of aggressive patients. Along the way I decided that I could either be benched by some withdrawing alcoholic, meth abuser, or I could learn to play through the pain and live my life.”
“As an ED RN you take care of many patients brought in by ambulance. On this day, I received a patient from EMS. I did my usual work of starting the triage process and then proceeded to get vital signs. When I explained the patient that I needed to take his blood pressure, he responded with “you can try.” Something about him told me to request assistance before moving any further. The police officer in the ED and other staff assisted with moving this patient to a room where seclusion could take place. When the officer asked the patient to comply he refused, so the officer cuffed one hand to the bed rail, when he suddenly grabbed a knife from inside his jacket. Thankfully, the wonderful officer on duty responded quickly and removed the knife from his possession. Sadly, just another shift in the ED.”
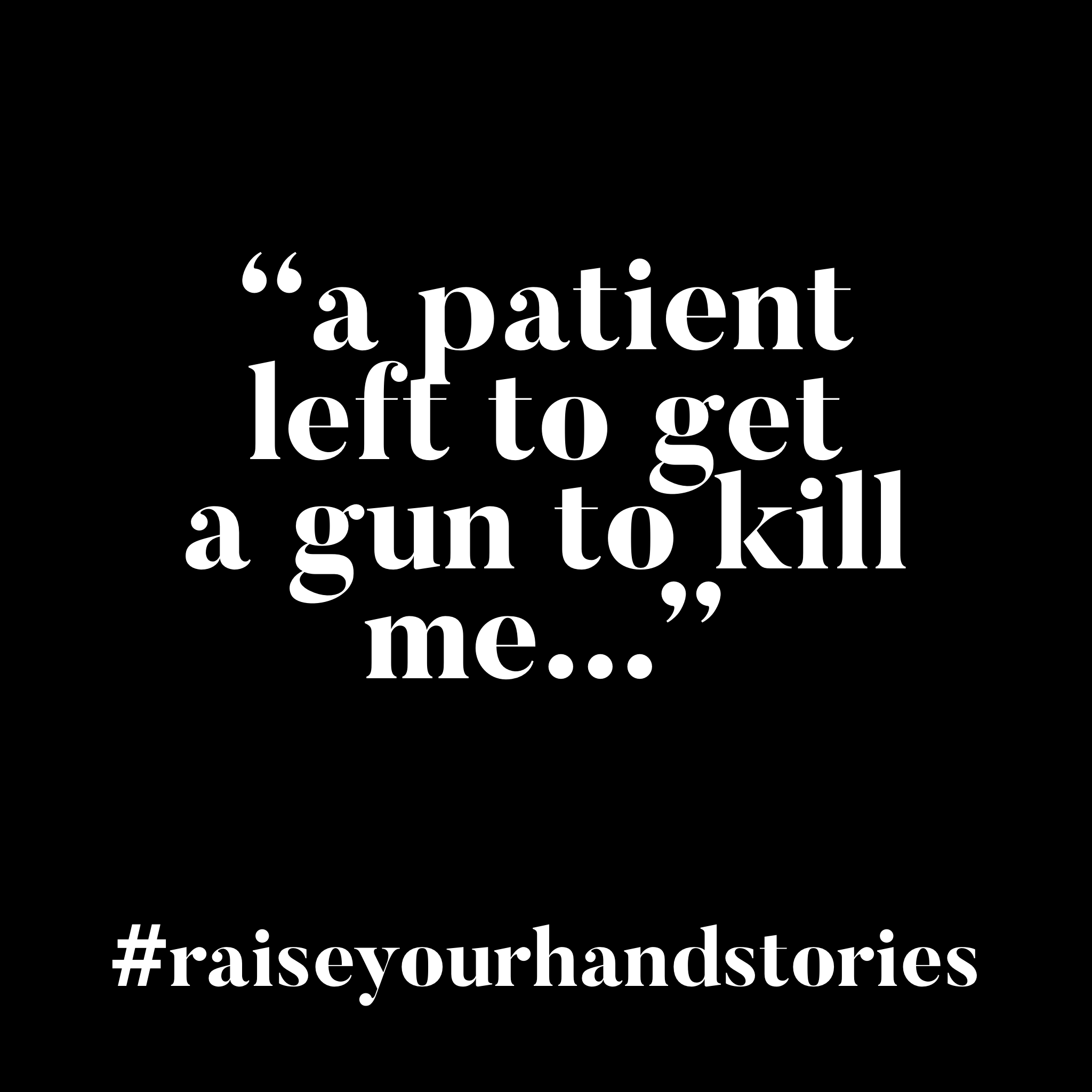
“ A patient left to get a gun to kill me and a physician but later was slap on the wrist. Attempted to strangle me, slammed against the wall. I was spit on and grab this patient pissed on me. This is just a few things in my 20 years.”
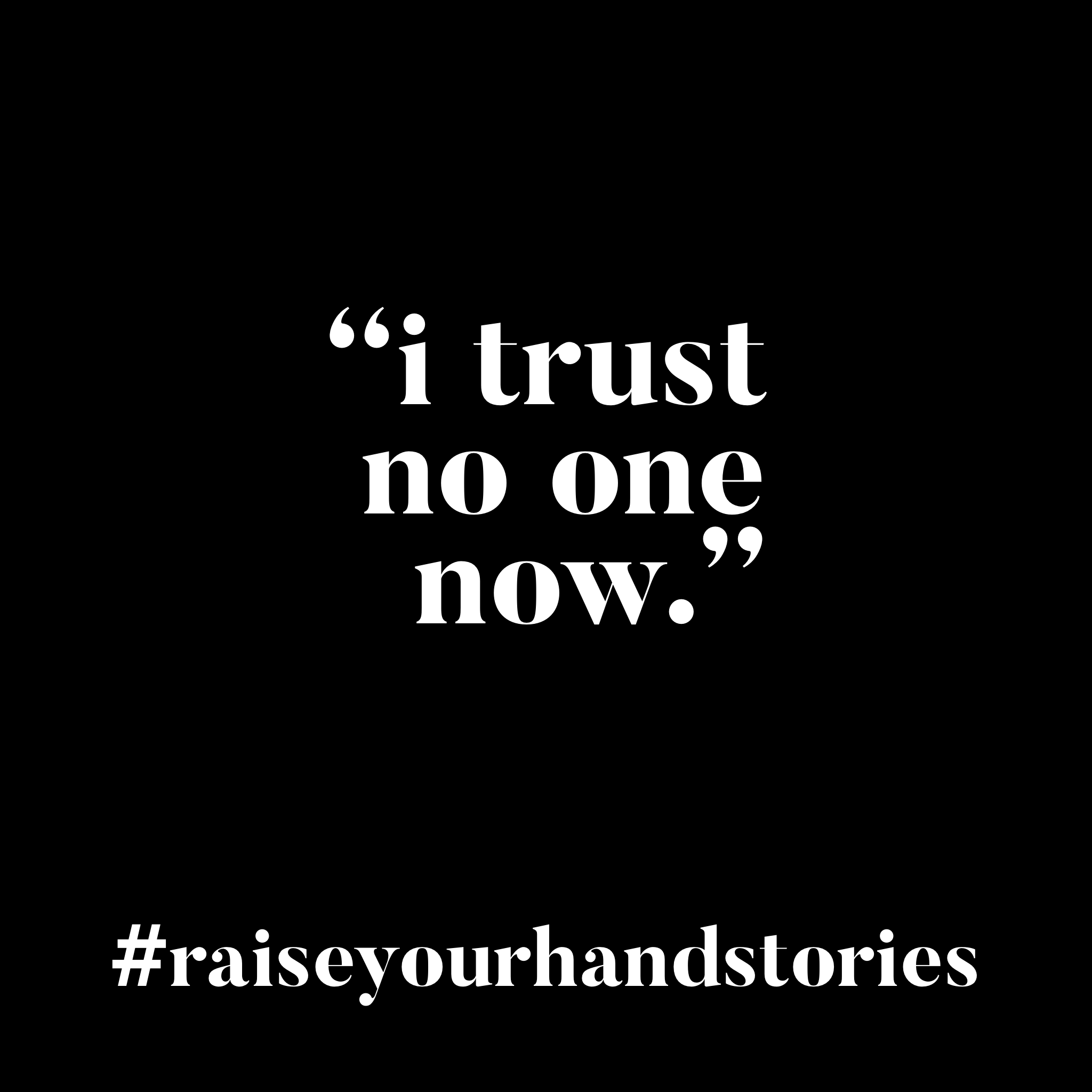
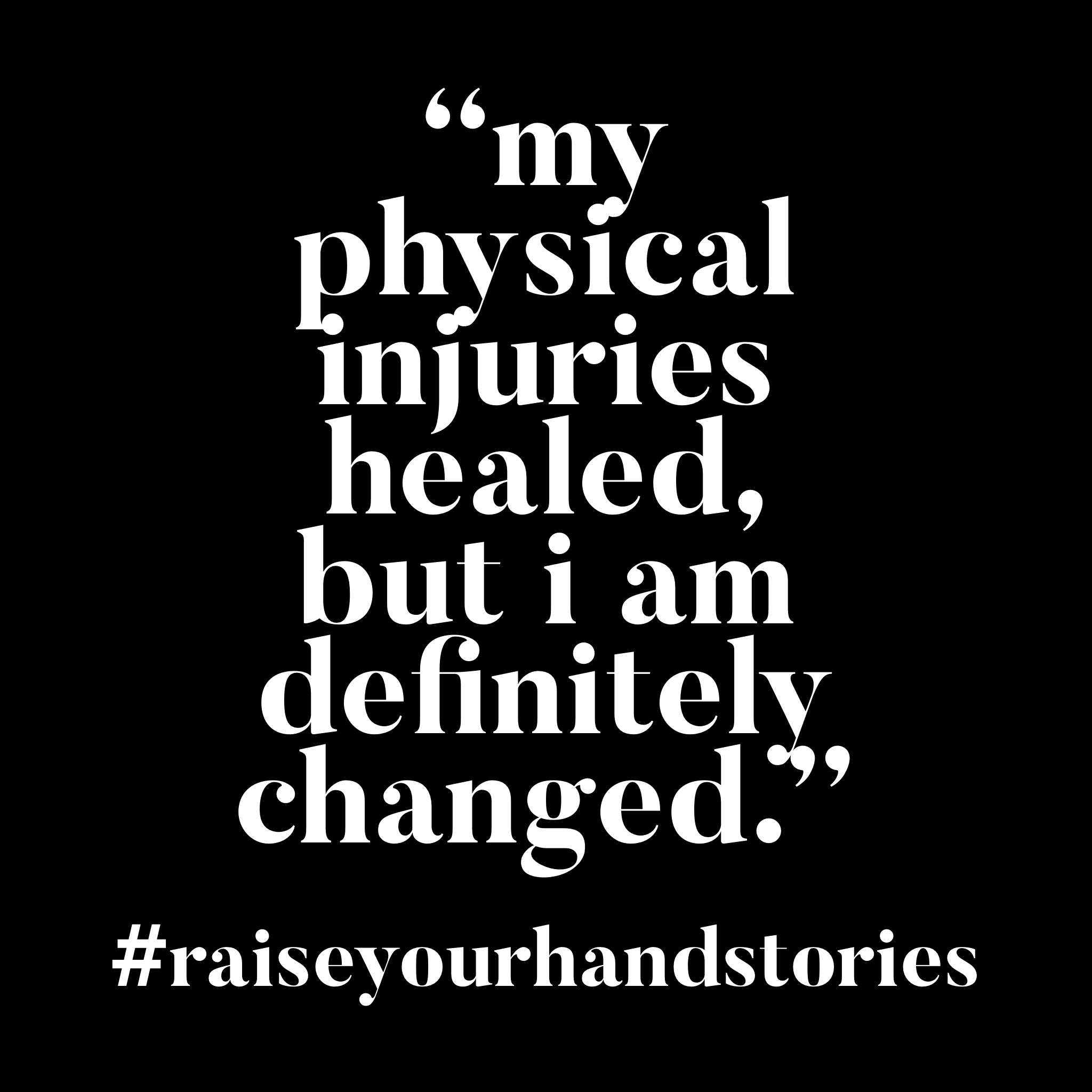
“I was violently assaulted this summer while on travel assignment. my physical injuries healed, but I am definitely changed. If it wasn’t for a few co workers who came to my aid, thing would have been so much worse. I was chased down the hall of the ER, knocked down, punched multiple times in the back of the head and they continued to stay on top of me hitting me and yanking my hair out until pulled off. I never saw it coming, I have been a nurse for 26 years and I know how to handle aggressive patients but this was different, I never even made it inside the room, this person just snapped. I never missed a day of work. I filed a police report but nothing came of it. I trust no one now...”
“I’d like to be the Poster RN for this campaign. I am still shocked at how poorly nurses get treated when injured from Workplace Violence.
It ended my career.
I was fired illegally.
I was kept from being able to use my LTD.
I lost my home in California.
I was send home to die wit hout care.
I was bullied by Workers Comp doctors.
Company Employee Health Nurse falsified the DWC1 report to assist in hiding injuries.
HR refused to help with getting LTD.
The director helped to hide the legal evidence.
The security director perjured himself in deposition. As did others.
I received much correspondence from nurses experiencing the same.
The path post injury from Workplace Violence is every bit as dangerous as the in-house ER violence. They would rather let you die than acknowledge and treat.”
“I was not a nurse but a PCA at the time. I was working night shift in the ER and it was a Friday night over the summer time. I was 6 months pregnant. It was the middle of my shift so around 3am. A very visibly drunk man came in with excessive vomiting via ambulance. He was already strapped down by his hands and his feet for being combative on the ambulance, so we followed the same existing procedures in the hospital as well. While strapping his hands to the bed, he was flailing and hitting nurses and doctors and I was pushed to the side to protect me and my pregnant stomach. After he was strapped down I was told to get his vital signs. Everybody else had left the room except for me and one of the nurses. I was taking his blood pressure when he was staring at my stomach and making comments about killing my baby. Nobody said anything back to him, myself included. He then proceeded to spit in my face. I was released to the bathroom to wash up. When I returned I was told that according to his chart he was positive for HIV/AIDS and Hepatitis C. I was overwhelmed with concern and stress and ended up having a panic attack and walking out that night. I felt sick. I felt like nobody at the hospital had my back. Nobody was as concerned as I was (yes I know that saliva is not a way to transmit these diseases) but I had a life inside of me that was just threatened verbally and then physically. So I left. I was called back into work the next day and told that since I walked out, I was put in a no rehire list and to turn in my ID badge. I lost my job at 6 months pregnant and put on a no rehire list because I felt unsafe and removed myself from a situation. I left healthcare all together after that. I guess I was just not cut out for it.”
“ My evening started off as I received report on my patients in the Emergency Room but the got a phone call from clinical supervisor to float to the 5 th floor. I went to the 5 th floor and before I received report on any patients I was told that my patient that I would not have needed a nurse right now. I went to her room where the [patient] was angry because of the previous shift nurse not taking care of her. At that point I tried to see what the issue was when she became irrational and threw herself to the floor saying she couldn’t breathe. Her family that was in the room began freaking out screaming to help her. I bent over the pt felt for a pulse and checked for breathing. Both were normal so I had a PCT help me get her back to bed. Once I got her into the bed the pt began threatening me about leaving and going to another facility because we were not managing her pain. I told her I could go look into her medication as I just got into floor and hadn’t even gotten report. That’s when she took her foot and kicked me in the upper abdomen into the air where I then landed approximately 20 feet away on my tail one striking my head on the wooden door of the room. I screamed and everyone came running. I was unable to get up immediately as I was stunned and hurt. They called a code behavioral and security came to floor. I however was escorted to the Emergency department where I was given a cat scan of me head and X-ray of my lower back and tailbone. While in ER I received pain medication due to the overwhelming pain in my tailbone. I had the police called and I did press charges against the wishes of the hospital. I was angry for what she did. I was out of work for almost 4 weeks and lost a good amount of pay because of this. I cried for days from pain as they sent me home with nothing to help. I spoke with the clinical supervisor a day later and she was not sympathetic at all due to me pressing charges. I had to go to the police department the day after with the help of my parents to make my official statement. She was arrested for assault but at the time it was still only a misdemeanor.”
“ I was in charge of the ER, in a level II trauma center located in an affluent area. A young man brought in by EMS, early 20’s, was combative from apparent drug use. Long and short of the story is that it took 10 firemen and nursing staff to hold the patient down to keep him from hurting himself. The end result was three firemen with body fluid exposure and one nurse with a bruise to the face. The police officers stated “well do you really want to file a report and ruin the rest of his life”. The PD was less than supportive and didn’t want to run through the process to properly charge the man for disorderly conduct and assault on 4 people. The executive leadership team was supportive of our actions, but the police did not support our desire to properly charge the assailant. Now our nurses don’t call the PD when they should because they feel like they won’t be taken seriously. The young man who assaulted the staff was a baseball player on scholarship at a division 1 school. The parents and PD “didn’t want his life ruined”. Yet three firemen had to be tested and put on precaution drugs for body fluid exposure protocol.”
“I have been verbally emotionally and physically assaulted over 10 times. The worst ever was an HIV patient who wanted to kill me by biting me multiple times. I suffered three bites and almost broke my wrist trying to get out if the room. I will never forget my boss had me clock out to go file charges against this family member of a patient. It took 3 long years and I had to take lots of time off from work without pay for court dates and on HIV prevention meds for 6 months. My attacker did get 2 years if jail time with 1 year suspended.”